Health
Testing fitness of aging brain

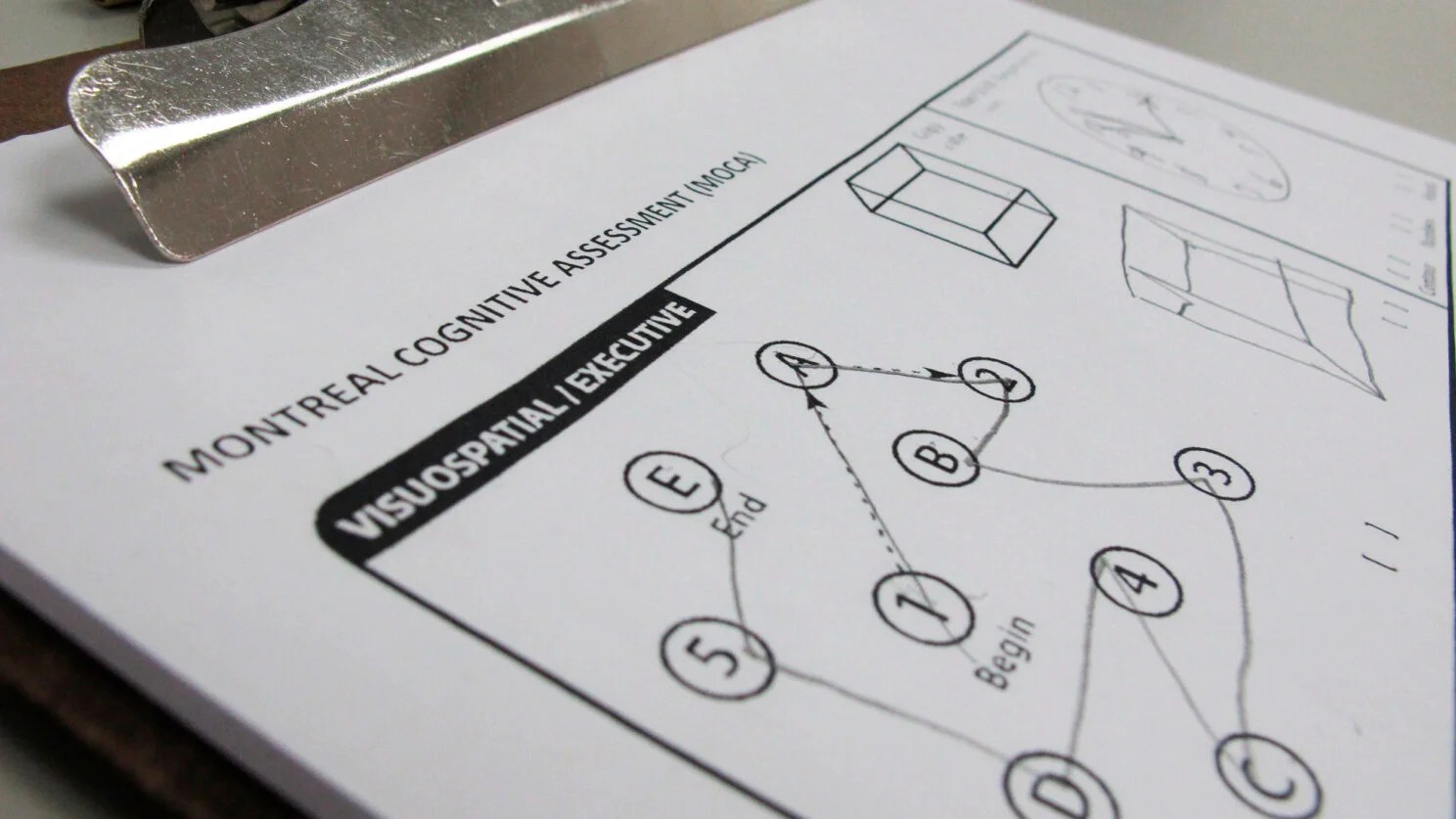
An example of the Montreal Cognitive Assessment test.
AP Photo/Allen G. Breed
Most voters back cognitive exams for older politicians. What do they measure?
Amid concerns about the mental fitness of the U.S. presidential candidates — Joe Biden is 81 and Donald Trump is 77 — some have called for mandatory cognitive tests for aging politicians. A recent poll showed 75 percent of voters favor such measures with support highest among the oldest cohort of Americans surveyed.
The Gazette asked clinical neuropsychologist Julie Brody Magid, Psy.D., clinical director of the McLean Memory Disorders Assessment Clinic and an instructor in psychology at Harvard Medical School, what functions cognitive tests measure, warning signs of mental decline, and how to maintain brain health. The interview has been edited for length and clarity.
What do cognitive tests assess?
Overall, cognitive tests assess a range of functions including memory, attention and concentration, language, spatial skills, orientation, and executive functioning. There are cognitive screening measures that offer a quick overview of different cognitive functions.
Currently, the most used cognitive screening test is the Montreal Cognitive Assessment, MoCA. In the past, the Folstein Mini Mental State Exam was frequently used by physicians. These are abbreviated cognitive screening measures that take five or 10 minutes to administer and score.
What does the MoCA test involve?
The MoCA test includes tasks that assess attention, orientation, naming of objects, learning a short list of words, and verbal reasoning tasks like analogies. It has a total score of 30 points. It’s a standardized test, given the same way every time. You earn a raw score based on your performance, which determines if your skills are within a normal expected range for your age and for your background. For example, given a person’s education and achievement, is their functioning where we would expect it to be? Or does the screening test show suggestions of a decline?

Sleep, exercise, and diet play key role in maintaining cognitive health, says Julie Brody-Magid.
Kris Snibbe/Harvard Staff Photographer
Who can perform well on the MoCA test?
There are very accomplished, smart people who can perform relatively well on a cognitive screening test like the MoCA even if they have had some changes in their day-to-day abilities. If you think of lawyers, doctors, or professors, it’s clear that they have strong intellectual ability, and what we call cognitive reserve, which is your cognitive savings account from being intelligent, educated, and enriched. Some people can “cruise” on their reserve even when they’re having subtle difficulties since their baseline abilities were so strong. Sometimes we might flag a patient who’s very high-functioning and who’s still performing relatively well on a MoCA test but may have subjective cognitive complaints. Some people come into my memory clinic saying, “Something’s not right, I’m not remembering well, I feel I’m declining.” They may notice themselves or the family may be observing changes. Those screening tests by themselves have some utility, but they don’t tell the whole story. The clinical information provided by the patient or family on interview about the course of change compared to who that person was at their highest level of functioning is very important. We need both sets of information to make distinctions about what a cognitive screening score means, and when further workup is needed.
What are the red flags that could warn of cognitive changes?
One red flag is if people are showing signs of rapid forgetting, such as if they are having a conversation, and something is discussed or planned, and minutes or hours later, they forget, and after being told again, they still forget. Rapid forgetting with repetitive questions is not usually an age-appropriate memory change. That type of memory change connotes Alzheimer’s disease, which is a disorder of memory storage or retention. Sometimes short-term memory loss can be accompanied by subtle language changes, where people can’t find words, especially when naming objects, they often will start to use generic words, such as “the thing,” “the whatchamacallit,” or they might describe the object, but they can’t name it. Those are some of the signs that we look out for.
“Rapid forgetting with repetitive questions is not usually an age-appropriate memory change.”
In vascular dementia, which is a risk factor for developing Alzheimer’s, we see more executive functioning issues, such as problems with organization, with keeping their paperwork in order; people lose track of the bills because they put them down somewhere or they don’t address them. We see people with vascular risk factors who have difficulty with reasoning and problem-solving. For example, they have a minor motor vehicle accident due to poor judgment and then don’t know how to handle it. Some people have reduced initiation and motivation; they stop doing things they always had passion for and cannot explain why. Slowed processing speed is often reported in daily functioning; everything takes much longer to work through and complete.
Is cognitive decline part of normal aging?
There are age-related changes that occur throughout our lifespan. As we age, there are some brain changes that occur as part of the normal aging process; white matter changes are the result of arteries that get narrowed or blocked by atherosclerotic plaque, this can begin around age 60. As that happens, there’s some associated slowing of processing, difficulty with being able to access information, pulling up that memory crisply, and efficiently finding words; some people identify those experiences as “senior moments.” We also have some cell loss and atrophy in the brain that occurs with normal aging. On neuroimaging, we see age-commensurate loss of volume in the cortex or gray matter, which plays a significant role in many functions including memory/learning and language. All of these changes are part of normal aging.
When is the right time to take a cognitive test?
What we typically suggest is that if a patient has what we call subjective cognitive complaints because they are noticing change, a cognitive screening should be done. However, one of the tricky parts of dementia, especially certain types like Alzheimer’s, is that the illness can affect the awareness center of the brain, and people don’t notice changes in themselves, but the family, spouse, or doctor notices change. If there’s any indication of subjective cognitive complaint or objective observation that that person is showing signs of early decline, that’s the time to pursue a neurocognitive screening test at minimum. That is often the beginning of the workup process, which can also include neuroimaging and bloodwork because other medical issues besides dementia can cause people to have cognitive problems.
Cognitive changes may be the result of hypothyroidism, anemia, a vitamin deficiency, sleep apnea, low blood pressure, unstable blood sugar, and a range of medical issues that can be reversible and allow the person to stabilize. Correction of vision and hearing problems can improve cognition too. Mental health issues like depression and anxiety can also affect cognition, but with appropriate targeted treatment, cognition can return to baseline. We must think holistically about all the factors that could contribute to somebody having cognitive issues to see which are treatable and potentially reversible.
What are the key steps to maintain our cognitive health?
There’s good research to support the Mediterranean diet for promoting successful aging and brain health. Exercise is very important because you are exercising the heart muscle and maintaining cardiovascular health. There are studies that show that exercise perfuses the brain with blood, which can cause neural growth and protection of key areas like the hippocampus. Exercise may delay the onset of cognitive symptoms or help prevent dementia. Studies of people with cognitive disorders have found that those who exercise perform better on average on cognitive tests and often do better in function than those who don’t exercise. Sleep is also very important for maintenance of cognitive health; at least seven to eight hours of sleep per night is necessary to clear debris out of the brain.
It is crucial to manage medical comorbidities like high blood pressure, high cholesterol, diabetes, smoking, sleep apnea, sedentary lifestyle, hearing/vision impairment, and depression. We also recommend limiting alcohol and marijuana use. We often see elderly people using excessive amounts of alcohol, which confers risk of cognitive decline and falls. There is literature to support that meditation and stress reduction promote brain health and cognitive functioning.
Other factors that promote brain health are engaging in activities that are stimulating to your brain such as doing crossword puzzles, learning a language, playing an instrument, discussing current events, and playing interactive games. Maintaining social connections and support is critical for mood stability and cognitive functioning.
Finally, it is very important to overcome the stigma associated with potentially losing your cognitive skills and reach out to get an assessment when you see the first red flags. If you let these problems go for too long, there are fewer modes of effective intervention. We have some good tools and resources available to support people’s functioning and manage symptoms and many more interventions are in the pipeline as we speak.