Medicare’s new power to negotiate drug prices will lead to an estimated $6 billion in savings for the federal government and a $1.5 billion reduction in out-of-pocket costs for seniors when the lower prices take effect in 2026, the Biden administration announced Thursday.
The negotiation program, which was authorized by the 2022 Inflation Reduction Act, has been a central talking point of the White House’s efforts to lower Americans’ cost of living, including for prescription medications, after inflation skyrocketed during President Joe Biden’s term. Vice President Kamala Harris is expected to continue campaigning on reducing drug prices in the runup to November’s election.
“It’s a relief for the millions of seniors that take these drugs to treat everything from heart failure, blood clots, diabetes, arthritis, Crohn’s disease, and more – and it’s a relief for American taxpayers,” Biden said in a statement.
The administration is scheduled later Thursday morning to release more information about the results of the negotiations with drugmakers, who have been trying – unsuccessfully, so far – to quash the program in federal court. However, officials are not expected to provide details about the cost cuts for each medicine.
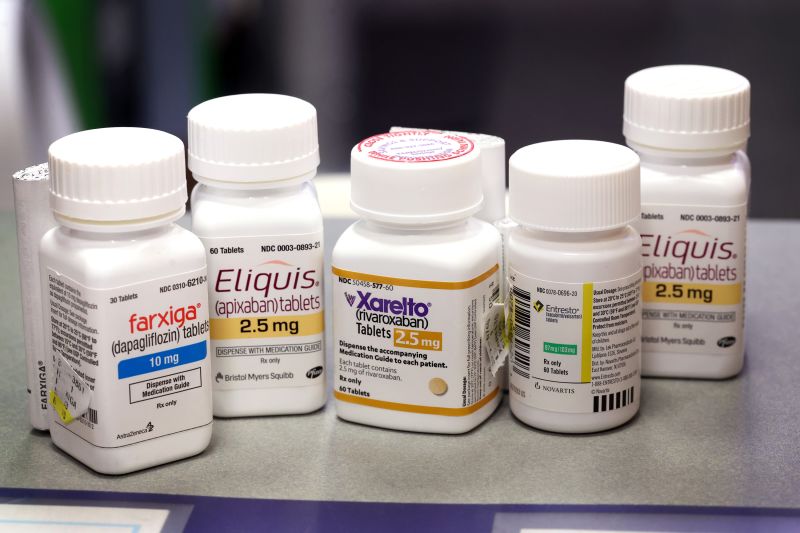
The initial round of negotiations focused on 10 of the most widely used and expensive drugs taken by Medicare enrollees. The medications are Eliquis, Jardiance, Xarelto, Januvia, Farxiga, Entresto, Enbrel, Imbruvica and Stelara, as well as Fiasp and certain other insulins made by Novo Nordisk, including NovoLog.
The $6 billion in savings estimate is based on Medicare’s 2023 cost for these drugs, Chiquita Brooks-LaSure, administrator of the Centers for Medicare and Medicaid Services, told reporters. The figure takes into account rebates and discounts provided to Part D plans by the drugmakers, or the so-called net price, according to the administration.
The Congressional Budget Office has estimated that the negotiation program will save Medicare $100 billion over a decade.
Many of the millions of Medicare enrollees who take the drugs subject to negotiation will see savings at the pharmacy counter, though it will depend on their Medicare Part D drug coverage, said Spencer Perlman, director of health care research at Veda Partners, a policy consulting firm for institutional investors. For many, medication costs are typically based on drugs’ list prices – before the rebates and discounts to the Part D plans – and those prices will be lower due to the program.
However, the benefit for enrollees will be muted by another provision of the Inflation Reduction Act – a $2,000 annual cap on out-of-pocket costs in Part D plans, which goes into effect in January. That will limit patients’ exposure to high drug expenses.
Drugmakers battle the law
The powerful pharmaceutical industry, which is not used to losing on Capitol Hill, has been trying to stop the negotiation process, filing multiple lawsuits in federal courts across the US contending that the program is unconstitutional in various ways. Several have said they were essentially forced to participate or otherwise face steep penalties or withdrawal from the Medicare and Medicaid markets.
But just last week, a federal district court judge in Ohio dismissed one of the challenges, marking the seventh loss in the legal battle by drug makers and their allies.
Although the drug manufacturers have repeatedly said that price negotiations will hurt their businesses and reduce innovation, several have indicated in recent earnings calls that the impact will be more muted.
“Now that we have seen the final price, we’re increasingly confident in our ability to navigate the impact of IRA on Eliquis,” said Chris Boerner, CEO of Bristol Myers Squibb, adding “I want to continue to emphasize that we firmly oppose government price setting under IRA.”
“While in the short term this might be manageable on our first set of drugs, in the long run, this policy is really not good for innovation [or] good for patients in the United States,” said Vasant Narasimhan, CEO of Novartis, which makes the heart failure drug Entresto.
The other manufacturers with drugs in the initial negotiations include Merck, Johnson & Johnson’s Janssen division, Novo Nordisk and AstraZeneca, among others.
Drugmakers are more concerned about the future rounds of negotiations, which will involve a larger number of drugs, some of which may not already come with hefty rebates, experts said.
“It’s much more of ‘We’ve now opened Pandora’s box of price negotiations’, and ‘Will this spill over to the commercial markets?’, which everyone thinks it will,” said Geoffrey Joyce, director of health policy at USC Schaeffer Center for Health Policy and& Economics.
The main industry lobbying group warned that the negotiation program – which it called “government price setting” – will harm research into new drugs.
“The IRA also fundamentally alters the incentives for medicine development,” Steve Ubl, CEO of the Pharmaceutical Research and Manufacturers of America, known as PhRMA, said in a statement, noting that companies are already changing their research programs. “Medicine development is a long and complex process, and the negative implications of these changes will not be fully realized for decades to come.”
The negotiation process
CMS considered multiple factors when developing its initial offer, including the drugs’ clinical benefits and the price of alternatives, among others. The agency also held listening sessions so patients and others could provide input on the selected drugs.
Health and Human Services Secretary Xavier Becerra told reporters that there was “substantial back and forth” during the negotiations.
“They had the opportunity to present their own proposed prices and to make counteroffers throughout the negotiation,” he said. “After substantial back and forth, either we accepted an offer or a company accepted our offer.”
After this initial round, Medicare can negotiate prices on another 15 drugs for 2027 and again for 2028. The number rises to 20 drugs a year for 2029 and beyond.
In the first two years of negotiations, only Part D drugs that are purchased at pharmacies will be included. Medicare will add Part B drugs, which are administered by doctors, to the mix for 2028.
CMS will announce the names of the drugs in the next round by February 1. The negotiated prices will take effect in 2027.